Two new studies add to the growing body of evidence that racism plays a key role in the persistent preterm birth disparities that exist between Black and white women in the United States.
While there’s ongoing research on the association between preterm birth and factors such as pregnant women’s health or level of access to medical care, there’s mounting evidence, including the two recent studies, that societal factors, including racism, also have an impact on the rates of premature delivery.
In a paper published in September, a workgroup convened by the March of Dimes looks at existing literature on contributors to racial disparities in preterm births and finds racism at the root of it all.
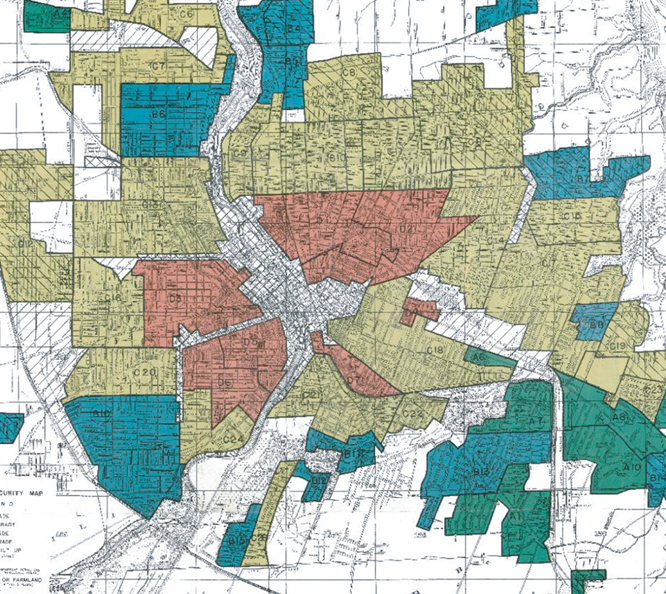
Meanwhile, in another study also published in September, researchers at the University of Rochester chose 15 zip codes in Rochester, New York, and overlapped them with the map of historic discriminatory home loan practice of redlining. Their findings show how structural inequality casts a long shadow in today’s health outcomes.
Preterm birth, which is delivery before 37 weeks of pregnancy, is associated with a higher risk of death and long-term health complications in babies. Researchers are interested in preterm birth rates because it is bellwether of a community or a nation’s health.
“Since there are many things that impact preterm birth, it likely captures both issues around access to health care and the resources we’re able to provide patients,” says Dr. Stefanie Hollenbach, an assistant professor of obstetrics and gynecology at the University of Rochester Medical Center. “But it also captures elements of the community and social structures that may be related to health outcomes.”
Preterm birth is on the rise in most countries and is now the second leading cause of death for children younger than five, after pneumonia, according to the World Health Organization. Every year, about 15 million babies are born prematurely around the world. That’s about one in 10 births.
In the U.S. preterm birth rates are no better than global rates: 1 in 10 babies are born too soon, according to the March of Dimes, a nonprofit education and advocacy organization for maternal and infant health. Preterm birth is the second leading cause of infant mortality in the U.S. and the leading cause of death among Black babies, according to the organization. Black women have the highest rate of preterm births compared with all other races and ethnicities in the U.S.
Below we explain the two new studies in more detail, including interviews with some of the authors.
Associations Between Historically Redlined Districts and Racial Disparities in Current Obstetric Outcomes
Stefanie Hollenbach, Loralei Thornburg, J. Christopher Glantz and Elaine Hill. JAMA Network Open, September 2021
In 2016, a local Rochester newspaper, the Democrat & Chronicle, ran a story about the newly-available redlining maps, which were digitized by a four-university effort called Mapping Inequality. Two researchers at the University of Rochester read the newspaper article and wondered if the maps may help with understanding how discriminatory loan practices decades ago are associated with health outcomes today, including disparities in preterm birth rates.
The practice of redlining began in the 1930s with the federal government’s Home Owners’ Loan Corporation. HOLC created color-coded maps that told banks where it was “safe” to issue home mortgages.
The maps had four categories or grades: Green for “best” neighborhoods, blue for areas that were “still desirable,” yellow for “definitely declining,” and red for “hazardous” areas. Areas that were marked “hazardous” mostly included low-income people, foreign-born individuals and, in most cases, Black people.
The practice lasted for three decades, but even after HOLC closed and Congress passed the federal Fair Housing Act of 1968 to ban housing discrimination based on race, religion and country of origin, the negative effects of redlining have persisted. Studies have shown that the practice has had long-lasting implications, not only affecting Black people’s socioeconomic status but also their health.
To explore their local community, the researchers looked at 64,804 birth certificates dated from 2005 to 2018 in 15 zip codes in Rochester, using the New York State Department of Health’s electronic birth certificate database. They then overlaid the data with the historic redlining maps. Some zip codes matched with a single redlining map designation and some included two or more designations.
They found preterm birth rates increased with worse HOLC color grades. The highest preterm birth rate —12.38% — was in the single zip code that overlapped with the area defined “hazardous” by HOLC map. The lowest preterm birth rate of 7.55% was found in a single zip code that overlapped with an area that was historically defined as “best” or “still desirable.” The overall preterm birth rate for the study population was 10.36%.
The associations persisted even after researchers controlled for levels of poverty and education and race of the parents.
They also found that the odds of being diagnosed with severe maternal depression and substance use disorder were significantly higher in areas that were labeled as “hazardous” compared with those labeled as “best” or “still desirable” in redlining maps.
“I think as clinicians, it’s important to recognize that there are so many facets to our patients’ lived experiences that are impacting their health outcomes,” says lead author Hollenbach. “All of us in the community, including physicians really need to be motivated to understand that health care is only one piece of it and our community structures are really impacting the differences as well.”
Even through the authors controlled for race, they didn’t do the analysis separately for Black and white women. As part of the study’s limitations, they also say that the results may or may not be generalizable to other U.S. cities.
“My hope is that this is the beginning of a long line of research with my colleagues where we can think about how to address persistent poverty in the Rochester area and whether some of the historic practices could be something that we can try to disentangle,” says co-author Elaine Hill, an economist and associate professor of public health science, economics and obstetrics and gynecology at the University of Rochester Medical Center. “I feel like we need to grapple with this history.”
Explaining the Black-White Disparity in Preterm Birth: A Consensus Statement From a Multi-Disciplinary Scientific Work Group Convened by the March of Dimes
Paula Braveman; et al. Reproductive Epidemiology, September 2021.
In 2017, the March of Dimes convened a multidisciplinary workgroup to review the existing literature on the persistent racial disparities in preterm birth in the U.S. The workgroup chair led a subcommittee in drafting an initial paper and subsequent revisions for members’ review. Revisions continued until consensus was reached, according to the paper.
The team looked at 456 peer-reviewed, English-language articles published in the past decade. “Limited web-based material from scientifically trustworthy sources [e.g., Centers for Disease Control and Prevention (CDC) reports] also were included,” they write.
Based on the metaphor of a river flowing from its upstream source to its downstream destination, the workgroup placed 30 potential factors leading to preterm birth intro three categories: upstream, midstream and downstream, depending on the proximity of their effects to preterm birth.
Downstream factors include prenatal care, substance use disorder, age and chronic conditions such as obesity, diabetes and high blood pressure. Midstream factors include stress, depression, social support, income, education and neighborhood socioeconomic disadvantage. The single item identified as the upstream factor was racism, which could directly and indirectly explain the disparities in midstream and downstream factors, according to the paper.
“No one of these downstream factors could explain the Black-white disparity by itself, but if you put them all together, they might,” says lead author Dr. Paula Braveman, a social epidemiologist, a professor of family and community medicine and founding director of the Center for Health Equity at the University of California San Francisco School of Medicine. “And then that raised the question: If you have so many biologically plausible [mechanisms], is there a common source that’s setting them in motion? And racism was the only factor that any of the members of the committee identified.”
The authors also looked at studies that explore the role of genes in preterm births and found that genetic factors at most may explain a small fraction of the disparity in preterm birth rates between Black and white women.
“When considering the potential role of genetic factors, it is important to note scientific consensus that race is primarily a social, not a biological, construct,” they write in their consensus statement.
The authors say that racism explains the racial disparity in socioeconomic factors. The legacy of slavery, 100 years of Jim Crow laws, racial residential segregation, and ongoing discrimination in employment, housing, policing and sentencing “have relentlessly deprived African Americans of socioeconomic opportunity,” they write.
Racial discrimination is also a powerful direct source of stress, researchers write. Stress can lead to changes to the body’s immune pathways leading to immune and inflammatory conditions, which are among the factors believed to be associated with premature delivery.
“What neuroscience has revealed, particularly over the last 10 to 20 years, is the enormous role that stress, and particularly chronic stress, plays in health through pathways that begin with neuro-endocrine disturbances that kicks into motion mechanisms that produce inflammation,” explains Braveman.
In short, the woman’s lived experience, including stress from racism, have already done a level of damaged that’s not going to be significantly reversed, she says.
“My hope would be that if [researchers and clinicians] read this review paper, it would make them more receptive to the notion that racism kills,” Braveman says.

Expert Commentary